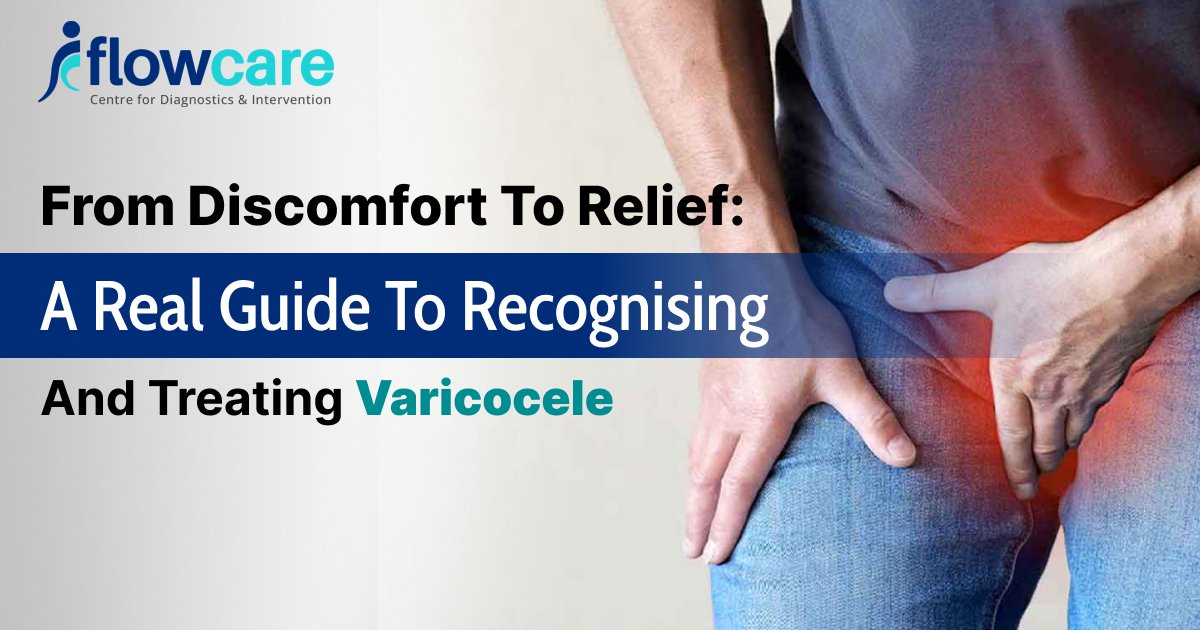
From Discomfort to Relief: A Real Guide to Recognising and Treating Varicocele
Are you experiencing testicular pain, swelling, or a strange heaviness? These could be early signs of varicocele.
This guide breaks down what a varicocele is, how to spot it early, and how to treat it effectively.
What is a Varicocele?
Varicocele is an abnormal enlargement of the veins in the scrotum caused by defects in the vein valves, causing blood to pool and hence the swelling.
These veins, called pampiniform plexus, help to cool the blood flowing through the testicles, which supports healthy sperm production.
Varicocele may disrupt this process, leading to infertility affecting upto 40% men(1).
Who is More Likely to Develop a Varicocele?
According to the study, approximately 15% to 20% of all adult males will have a varicocele, which impacts male fertility, testicular health, and overall confidence(2).
Certain factors may increase the risk of developing it. Knowing these may help you stay informed and get timely care if required.
- Age
Varicocele may develop during puberty or early adulthood, most commonly between the ages group 15 and 25.
These are the growth years leading to increased blood flow in the scrotum.
- Genetics
Genetics also play an important role.
If anyone from your family has a history of venous valve weakness or infertility due to varicocele, there is a chance that you might develop it too.
- Height and Body Type
Generally, tall men with a lean body type have a higher risk of developing varicocele as compared to others.
The exact reason is unknown, but it can be related to blood flow against gravity in the scrotal veins.
- Physical Activity and Strain
Frequent heavy lifting, intense physical exertion, or chronic constipation (causes straining) may worsen the already existing vein issues and increase the chances of varicocele.
- Left Side Dominance
Due to anatomical differences, 78%-93 % of cases of varicocele are located on the left side. (3)
- Standing for Long Hours
Job or routines that require long-standing hours might lead to varicocele due to altered blood flow in the scrotal veins, especially when combined with other risk factors.
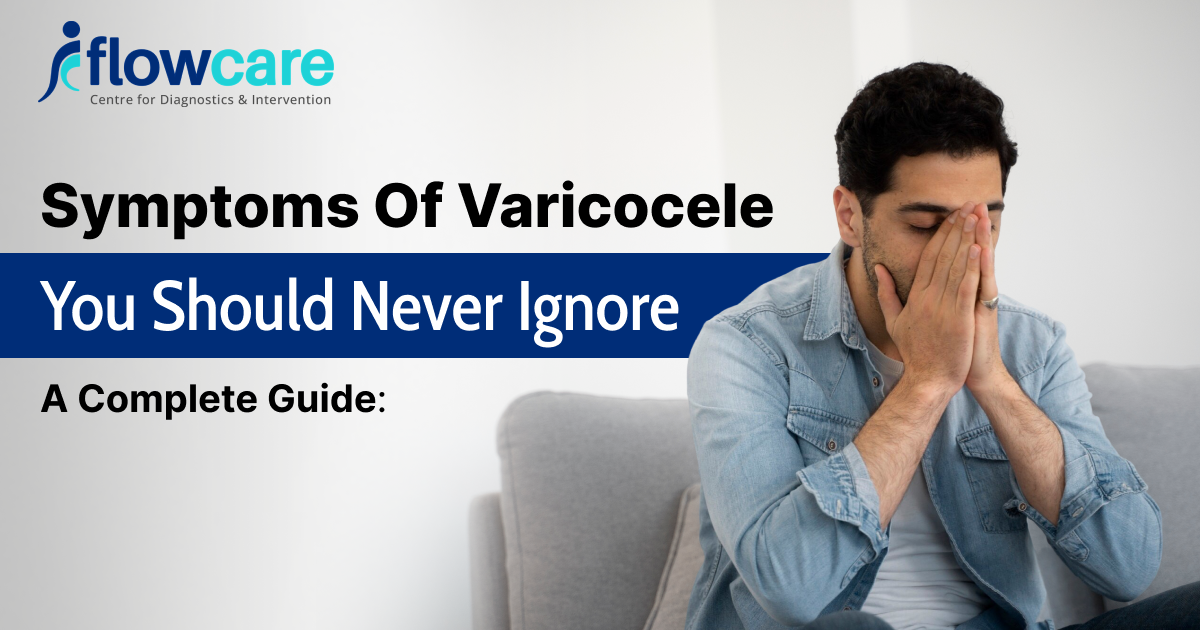
How Do You Recognise a Varicocele?
Identify Common Signs and Symptoms
The condition is often asymptomatic, and many people may develop it only during a routine checkup or fertility assessments.
Some of the signs that can help you know if you have a varicocele are:
Visible/Palpable Signs:
- A mass or lump in the scrotum is often called a “bag of worms” appearance.
- Noticeable vein or swelling above the testicle, primarily on the left side.
Pain or Discomfort:
Dull ache or heaviness in the scrotum may worsen by standing, hot weather, or heavy physical activity. It often becomes better while lying down.
Testicular Atrophy
Varicocele may lead to small testicles or shrinkage due to prolonged impaired blood supply.
Fertility Issues
Reduced sperm count, motility, quality, and occasionally low testosterone levels.
When to See a Doctor?
If you notice a lump, consistent pain, or itching, changes in the size of the testicles, or infertility, seek immediate medical attention for a thorough evaluation.
How does a Doctor Diagnose Varicocele?
Clinical Examination
Physical examination is done in the standing position, since the forces of gravity increase the prominence of a varicocele.
A subtle varicocele can be recognised with the help of the Valsalva manoeuvre (breath holding and bearing down).
Imaging and Grading
Ultrasound: Confirms diagnosis, measures vein size, evaluates blood flow, and helps grade severity.
Grading:
1) Grade I: Small, not visible, only palpable with Valsalva manoeuvre.
2) Grade II: Palpable without Valsalva, not visible.
3) Grade III: Large, visible bulging veins
How to Treat Varicocele Effectively?
The following are the treatment options available to treat the condition effectively:
Surgical Treatment
- Microsurgical Varicocelectomy
The gold standard of varicocele repair
This is done under an operating microscope, and each abnormal vein can be identified and ligated accurately, with lymphatics and arteries preserved.
Has a low recurrence rate and the least risk of complications
Performed under local or general anaesthesia, the patient does not have to stay admitted until recovery is completed.
- Laparoscopic Varicocelectomy
Keyhole surgery, which involves small incisions in the abdomen, is performed together with camera-guided surgery. It is performed under general anaesthesia.
Laparoscopic Varicocelectomy is faster to recover than open surgery, with slightly more recurrence and complication rates than microsurgery.
It may be used preferably in bilateral varicoceles or situations requiring abdominal exploration.
- Open Surgery (Inguinal or Retroperitoneal Approach)
A conventional surgical approach, which is nonetheless applied in certain centres where the capability of microsurgery is lacking
It is associated with greater dissection and risks of complications, including hydrocele development or destruction of adjacent structures.
Usually, it takes longer to heal.
Source:ncbi(4)
Non-Surgical Interventions
The procedure involves less invasiveness and is assisted by imaging and is done by a radiologist.
The procedure starts by inserting a catheter into a vein ( in the groin or neck).
The catheter is then directed to the leaking testicular vein and fills it with coils or sclerosing substances to block it, thus preventing back flow.
The recovery time is short – most patients start their normal activities within 24 hours.
Varicocele embolisation is especially useful for individuals who are not willing to go for surgery, who are seeking to get enrolled in the army or have a recurrence of varicocele even after multiple surgical interventions.
When is the Treatment Required?
Not all varicose veins require interventions.
Treatment is necessary when there is:
- Pain and discomfort
- Infertility
- There is evidence of testicular atrophy or poor testicular development (especially in adolescents)
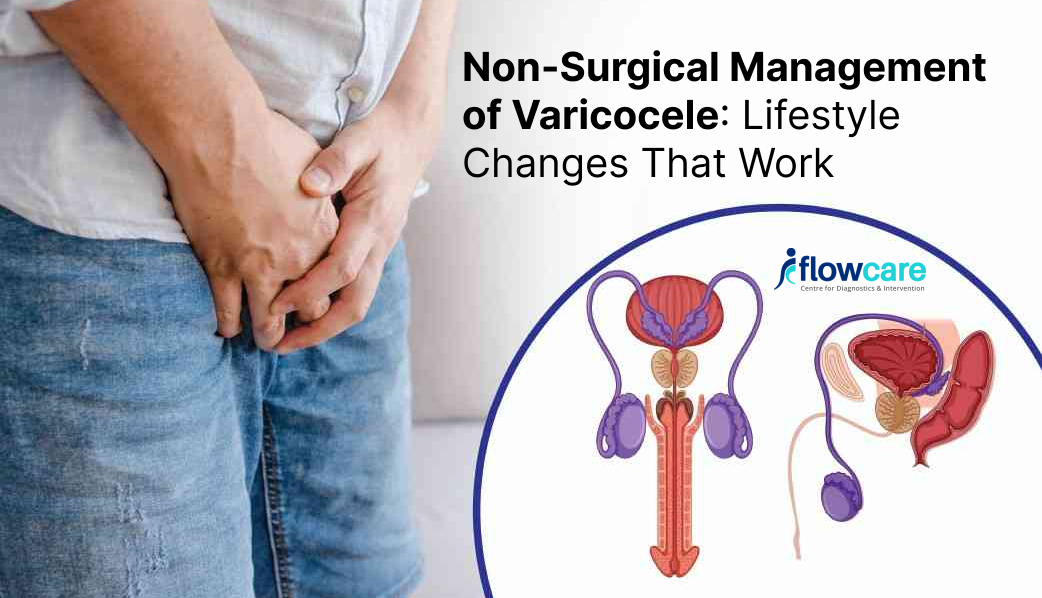
What Lifestyle and Supportive Measures Should be Taken?
Patients with mild symptoms can take the help of these methods to avoid condition progression:
- Wearing a supportive garment
- Avoid heavy weight lifting and long standing hours
- Maintaining weight
- Avoid hot showers
- Or taking pain-relieving tablets
- Avoid smoking and alcohol
These measures can help reduce the discomfort or avoid the condition, but cannot permanently cure a varicocele.
Conclusion
Although most people do not know it, the condition of varicocele is prevalent.
It may not lead to a noticeable condition, but it can undermine your fertility, comfort, and health in general when neglected.
Varicocele is manageable or can be cured if proper medical assistance is taken and certain lifestyle changes are made.
In case you have experienced testicular pain and swelling or you are experiencing some problems connected with fertility, you should not be afraid to approach a doctor.
The first step to diagnosis might create the most significant difference in your life regarding your well-being.
FAQs
What is the best way to treat a varicocele?
Microsurgical varicocelectomy and varicocele embolisation are effective techniques with good & proven outcomes to treat the condition.
However, embolization is often preferred because it is minimally invasive and offers a shorter recovery period.
How to self-identify a varicocele?
You will find a lump or dilated veins in the scrotum, which can resemble a “bag of worms”.
Other indications are dull pains, dull heaviness, and discomfort exacerbated by standing and relieved by lying down. A doctor should always be consulted to clarify.
How do you identify the stage of a varicocele?
Ultrasound is often used to assess varicocele’s grade, severity, and blood flow.
Is grade 3 varicocele curable?
Yes, Grade 3 varicocele can be fixed and frequently cured, particularly through an operation, such as microscope-aided varicocelectomy / or embolisation.
The treatment can reduce symptoms, enhance fertility, and prevent other complications.
Can yoga cure varicocele?
Yoga can not treat varicocele, but it can be useful when the symptoms are mild, such as discomfort or help with blood circulation.
Yoga poses can relieve pressure on the scrotum (such as Legs-Up-the-Wall). Medical treatment is, however, required to fix the underlying vessel problem.