Ultrasound/CT-Guided Fine Needle Aspiration (FNA), Biopsy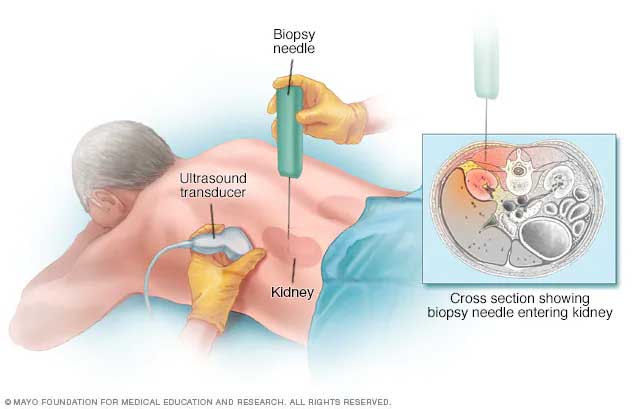
Ultrasound/CT-Guided Fine Needle Aspiration (FNA), Biopsy has almost replaced the more invasive surgical biopsy. Under local anaesthesia, an expert Interventional Radiologist using Ultrasound/CT Imaging guidance inserts a very fine and hollow needle through the skin into the mass from which the sample needs to be taken.
Tissue sample can be taken from any visceral organs like liver, renal, pancreas, abdominal mass, lung mass or prostate to make a diagnosis and plan further management/treatment. This procedure is very reliable and carries a very low risk profile.
The sample thus collected is sent for evaluation. The recovery period is very short and the patient is able to resume the normal activities soon.
Liver Abscess:
An abscess is a collection of infected fluid within the body and most commonly seen as liver abscess. Rapid diagnosis and treatment of liver abscesses is vital, otherwise it can be life-threatening. In earlier days, surgical drainage was the only treatment available for this condition; however, novel Interventional Radiology treatment knows as Percutaneous Catheter Drainage (PCD) or Needle Aspiration (PCNA) have been proven to be worthy alternatives of surgery.
Percutaneous Drainage of liver abscesses can be undertaken by either PCD or PCNA technique. Usually for smaller liver abscesses (less than 5 cm) PCNA is undertaken, but for larger liver abscesses PCD technique is more successful. Benefits of Percutaneous Drainage over Surgical Drainage include shorter recovery period, no need for general anesthesia, reduced cost, greater success rate.
Percutaneous Needle Aspiration is performed under real-time Ultrasound guidance during which a very thin needle is advanced into the abscess cavity and the abscess contents are aspirated (sucked) in an attempt to completely empty the abscess cavity.
In case of Percutaneous Catheter Drainage, under ultrasound guidance, a catheter is placed in the abscess cavity to gradually drain the contents into the collection bag attached to the catheter. The catheter will remain in place till the abscess fluid has stopped draining and the infection has subsided, which may take up to 5-7 days.
The main benefit of Percutaneous Drainage of Liver Abscess is that no surgical incision is required, just a small hole in the skin that might even not need stitches. Recovery period is also significantly faster than that of the surgical drainage.
Transrectal Ultrasound-Guided Biopsy (TRUS Guided Biopsy)
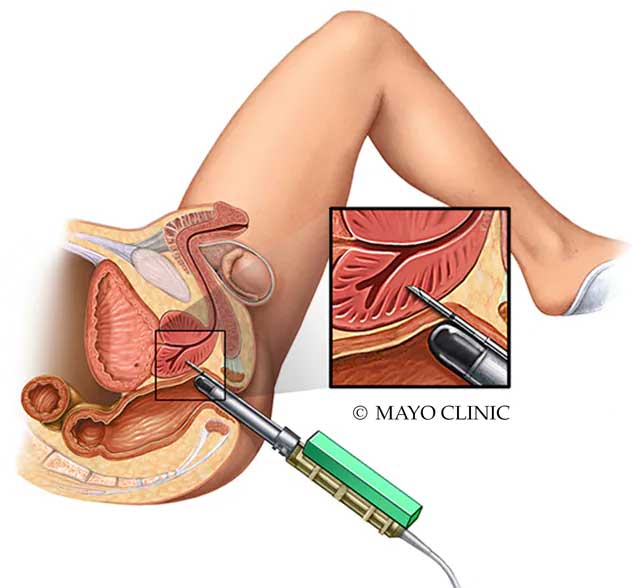
TRUS-Guided Biopsy of prostate is widely acclaimed as the mainstay procedure in the diagnosis of prostate cancer. TRUS-Guided Prostate Biopsy is used to collect samples of prostate gland tissue to look for cancer cells without the need of any incision/cut in the skin.
This procedure is usually done with the patient being given local/regional anesthetic. With the patient lying on his left side, the expert Interventional Radiologist inserts an Ultrasound probe into the patient’s rectum to examine the prostate. A very thin fine needle is pushed along the Ultrasound probe and advanced into the prostate gland to collect the tissue sample. This procedure is repeated in order to collect different tissue samples and might take up to 20-30 minutes.
After the procedure, the patient is observed for some time and once stable, is discharged on the same day. A follow-up is then scheduled to look upon the test results.
Bone Marrow Aspiration
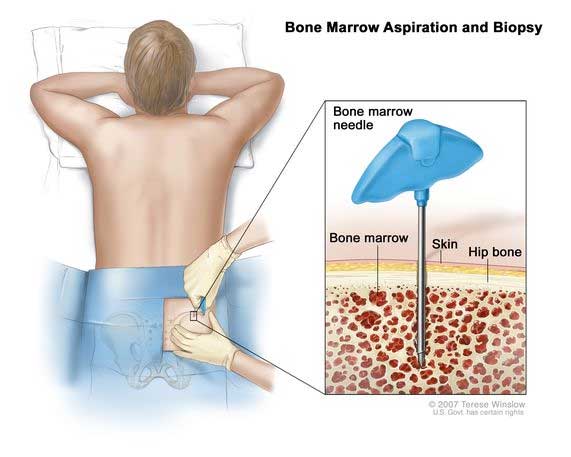
Bone Marrow is the soft tissue inside in the hollow part of most bones that assists in formation of blood cells. Bone Marrow Aspiration is the procedure to take a small sample of the liquid part of this tissue for examination that helps in identification and monitoring of progression and/or treatment of blood-related diseases such as anemia, myelofibrosis or myelodysplastic syndrome, leukopenia, leukemia (blood cancer), multiple myeloma, lymphoma, hemochromatosis, tuberculosis, Gaucher’s disease or amyloidosis, etc.
This procedure is usually done under local/regional anesthesia to the area from where the aspiration is to be performed (generally pelvis or chest bone). Once the patient is made comfortable, the expert Interventional Radiologist inserts a hollow needle through the skin into the bone and aspirates (through suction) a small amount of bone marrow tissue. The needle is then removed and a dressing is applied to the skin. Typically, the procedure is completed under 30 minutes.
After the procedure, the patient is observed for some time and once stable, is discharged on the same day. The bone marrow tissue sample is sent to the laboratory for examination.
Transjugular Liver Biopsy (TJLB)
Liver Biopsy is the procedure to obtain a small sample of liver tissue in order to diagnose a liver problem, to determine the severity of liver disease (staging) and to plan and monitor the progress of treatment. Also, in case of liver transplant, liver biopsy is obtained to assess the functioning of the liver.
Transjugular Liver Biopsy (TJLB) is an advanced pinhole technique that is safe in patients who have liver issues with deranged coagulation profile and not suitable for percutaneous needle biopsy. This procedure is performed under local anesthesia and almost a painless procedure. This is a very safe procedure with very minimal risks when performed by an Experienced Interventional Radiologist.
The patient is given local/regional anesthesia and then a flexible catheter (plastic tube) is inserted into the Jugular Vein (Veins in the neck) through a very small pin hole. Under real-time X-ray Guidance, the catheter is then advanced into the Hepatic Vein (the large veins that carries blood from the liver to inferior vena cava). Then a contrast dye is injected which helps to identify/confirm the correct placement. Once the correct placement is confirmed, a biopsy needle is advanced through the catheter and into the surrounding liver tissue through the Hepatic Vein. Once the liver tissue sample is collected, the biopsy needle and the catheter are pulled back and a bandage is applied to the skin incision.
After the procedure, the patient is observed and once stable, is discharged on the same day.
Percutaneous Transhepatic Biliary Drainage (PTBD)
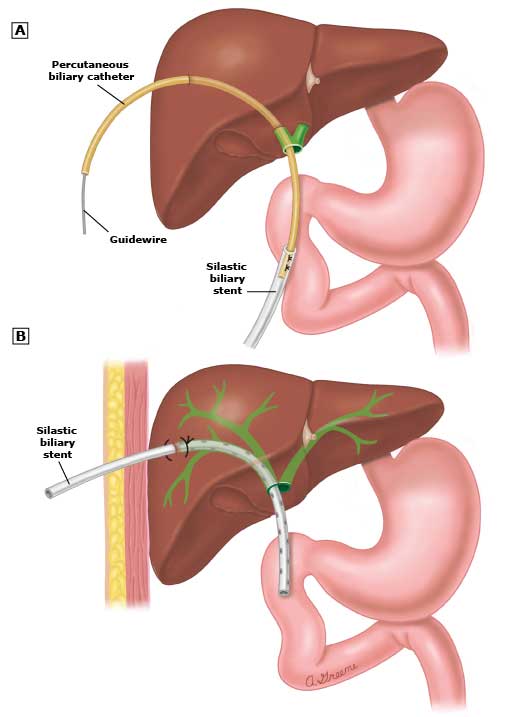
Percutaneous Transhepatic Biliary Drainage (PTBD) is a minimally-invasive procedure in which a Biliary Drain (small, flexible, plastic tube) is placed through the skin into the liver in order to drain bile and relieve the pressure in the bile ducts caused by a blockage. This is a very safe technique and carries a very low risk profile.
It is done in the patients who are having blockage in bile duct due to cancer or stone where endoscopic drainage is not possible or in failed ERCP.
Under local anaesthesia and ultrasound guidance, an expert Interventional Radiologist punctures the peripheral bile duct and once the bile starts pouring, a guidewire is pushed into system under x-ray guidance. The bile can be drained externally into a collection bag (drainage bag) as well as internally in the digestive tract (duodenum-small bowel) depending on the circumstances. In the patients who have advanced disease, a self-expanding metallic stent (SEMS) is placed for better drainage.
After the procedure, the patient is kept under observation for some time. Once stable, the patient can be discharged with appropriate instructions and follow-up.




