I. Introduction
Having a headache for at least 15 days a month, consistently, for at least three months, is considered chronic. It has a major effect on one’s day-to-day life and general quality of life. Accurate diagnosis and management of persistent migraines need an understanding of their causes. This blog defines chronic headaches, classifies the various chronic migraines, and discusses potential triggers for chronic headaches.
Types of Chronic Headache:
Chronic Migraine:
Migraine-like headaches that linger for at least 15 consecutive days per month for three months or longer are considered chronic migraines. Pain, sensitivity to light and sound, and visual abnormalities called auras are common migraine symptoms.
Chronic Tension-Type Headache:
The most common kind of persistent headache is tension-type headache. Both sides of the head or neck are experiencing constant, numbing, terrible agony. Anxiety, stress, and muscular strain may all play a role in triggering or exacerbating migraine attacks.
New Daily Persistent Headache (NDPH):
For those who have never suffered from migraines before, a new daily persistent headache (NDPH) is a severe kind of chronic headache that may strike at any time and last for months or years. In most cases, the pain is relentless and ranges from mild to excruciating.
II. Causes of Chronic Headache:
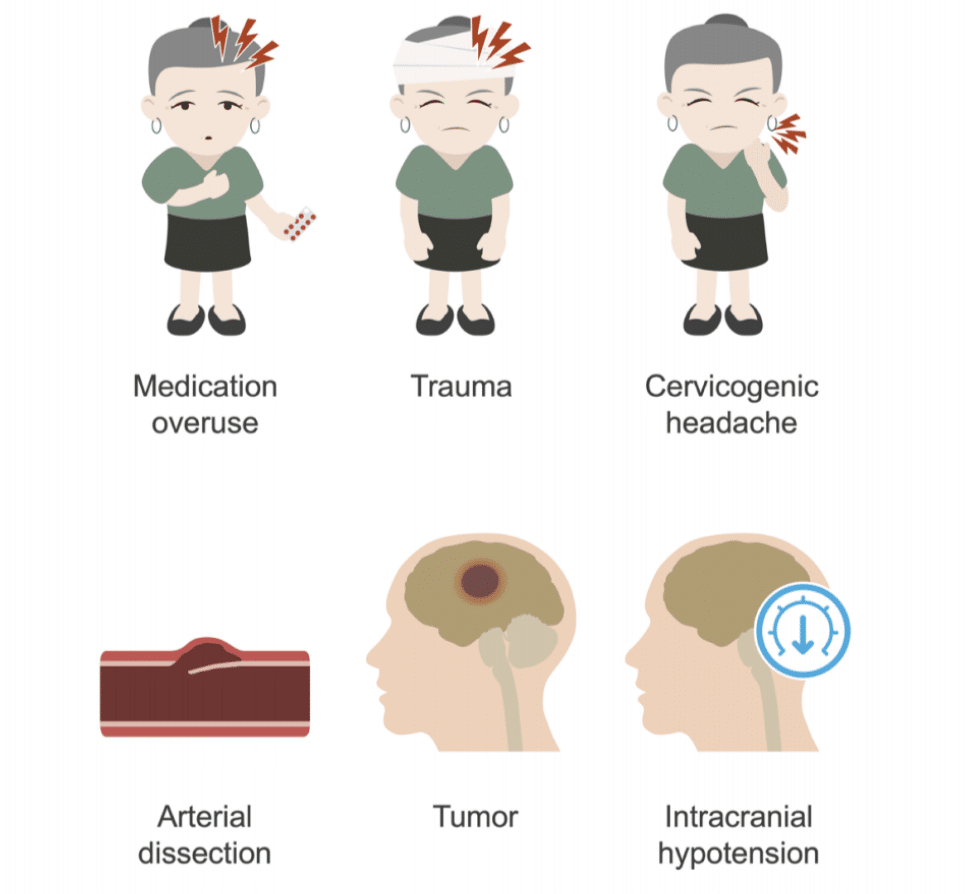
It’s not always clear what triggers persistent migraines, although there are a variety of potential explanations. Common reasons consist of:
Illness:
Chronic migraines are often caused by infections, sinusitis, or other serious conditions. Giant cell arteritis and meningitis are two inflammatory illnesses that may produce ongoing headaches in humans.
Stress:
Stress headache is a common risk factor for chronic migraines. Emotional stress, tension, worry, and even depression may trigger or intensify chronic migraines.
Environment:
Exposure to loud noises, strong odors, bright lights, or sudden changes in weather may all trigger migraine attacks in those who are prone to them.
Genetics:
The probability of acquiring persistent headaches may be increased if there is a family history of headaches or migraines. The brain’s perception of pain and its reaction to various stimuli may be influenced by a person’s genetic makeup.
III. Symptoms of Chronic Headache
1. Prodrome:
The prodrome phase of a persistent headache begins hours to days before the onset of the headache itself. During this time, people may notice small changes in their mood, actions, or bodily sensations.
2. Aura:
Some people who suffer from persistent headaches report seeing an aura before or alongside the onset of the headache. The neurological condition known as aura may take several forms of sensory disruption.
3. Headache:
The pain episode is the most noticeable and debilitating aspect of persistent migraines. In this stage, you’ll have a severe, ongoing headache in back of head that may continue for many days. It’s usually only on one side, although it might affect both.
4. Postdrome:
After the headache has faded, a person may experience the postdrome phase, sometimes known as the “headache hangover.” During this time, people may feel exhausted and drained, and they may still be experiencing some lingering symptoms.
IV. Diagnosis of Chronic Headache
1. Detailed Medical History:
Chronic migraines can only be diagnosed after a thorough examination of the patient’s medical history. The doctor will probe into the headaches’ pattern, length, severity, and any other symptoms the patient has noticed.
2. Physical Examination:
The healthcare professional will check the patient’s vitals, including blood pressure, pulse rate, and neurological reflexes, as well as their general physical condition. The head, neck, and spine may all be checked for tension or anomalies that might be contributing to your migraines.
3. Neurological Evaluation:
Conducting a complete assessment of the nervous system might help pinpoint the underlying cause or causes of recurrent migraines. Sensory abilities, reflexes, motor skills, and physical strength might all be tested.
4. Imaging Studies (MRI or CT scans):
Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scans may be indicated to rule out structural issues in the brain that might be causing the persistent migraines in certain patients. These scans may be helpful in identifying illnesses like cancer and vascular problems that need targeted care.
5. Headache Classification:
Chronic headaches fall into a wide variety of classifications, each with its own set of symptoms and set of potential reasons. Headache management helps doctors determine what kind of headache a patient has, which is important for treating the condition effectively. Common types of persistent headaches include tension headaches, migraines, cluster headaches, and headaches brought on by using too many painkillers.
V. Treatment of Chronic Headache:
1. Lifestyle Changes:
Lifestyle changes may have adverse effects on the frequency and intensity of chronic migraine attacks. Adopting a regular sleep pattern, controlling stress with relaxation methods, eating a healthy, well-balanced diet, and avoiding known headache triggers like alcohol, caffeine, and certain foods are all good places to start.
2. Pain Medications:
OTC pain medicines including acetaminophen, ibuprofen, and aspirin may help with mild to severe migraine symptoms. But regular or heavy usage might cause medication-overuse migraines, so it’s important to take these drugs exactly as prescribed.
3. Triptans:
Migraine sufferers may use triptans, a special family of drugs created to alleviate their pain. They work by narrowing blood arteries and blocking pain signals in the brain. Headache tablets, nasal sprays, and even injections are just some of the triptan delivery methods available.
4. Preventive Medications:
Chronic migraines may be brought on or made worse by stress and tension. Stress management and headache remedies may be achieved by the use of a range of relaxation methods, such as deep breathing exercises, progressive muscle relaxation, meditation, and biofeedback.
5. Relaxation Techniques:
People who suffer from persistent migraines should work closely with their doctors to come up with an individualized treatment strategy. Migraine therapy varies from case to case and patient to patient based on a number of factors.
6. RFA treatment
Using radio waves’ electrical currents to numb painful nerves is a nonsurgical method known as radiofrequency ablation. In order to prevent pain signals from reaching your brain, electrical currents burn your nerves.
7. Nerve block treatment
Common migraine headache treatments include nerve blocks. In order to prevent some nerves from transmitting signals to the brain during the treatment, a medical practitioner injects a nerve-numbing chemical around certain nerves. This may prevent someone from feeling the discomfort that comes with migraine headaches.
VI. Prevention of Chronic Headache:
1. Identify Triggers:
Track your headaches in a notebook so you can identify trends and causes. Common allergy triggers may include specific foods (such as processed meats and aged cheeses), hormonal shifts, environmental variables (like strong odors or bright lights), stress, and lack of sleep. A person’s vulnerability to acquiring chronic headaches may be mitigated by the recognition and avoidance of headache triggers.
2. Maintain a Regular Sleep Schedule:
Maintaining a regular sleep routine is crucial for migraine avoidance. Maintain a consistent bedtime and wake time of 7 to 9 hours every night. Migraines are often brought on by disruptions in sleep routines that disrupt the body’s natural circadian cycle.
3. Stay Hydrated:
Staying hydrated during the day is especially crucial if you suffer from migraines since dehydration is a known trigger. Limit your intake of caffeinated and sugary drinks, and increase your water intake instead.
4. Manage Stress:
In addition to the other symptoms, cluster headaches are often triggered by stress. Yoga, meditation, deep breathing exercises, and time spent in nature are all great ways to de-stress. Migraine headaches may be avoided with the use of stress management techniques.
5. Limit Caffeine and Alcohol:
Try to cut down on the coffee and booze. Migraines may be brought on by both coffee and alcohol. In times when you’re more likely to have headaches, cutting less on these things might help.
VII. When to Seek Medical Attention:
Although most migraines are mild and respond well to dietary and nonprescription drug management, certain symptoms do need seeing a doctor. Seek medical treatment immediately if any of the following symptoms develop:
- A very intense and sudden headache (sometimes known as a “thunderclap headache”).
Symptoms include a high body temperature, stiff neck, disorientation, and/or convulsions accompanying a headache.
- Headache symptoms that have never been experienced before
- Weakness, paralysis, difficulty speaking, or altered vision in addition to the headache.
- Patients with a history of cancer or autoimmune illnesses often suffer from a unique kind of headache.
VIII. Conclusion:
Accurate treatment and preventative actions are essential for chronic migraine management. Preventing headaches requires knowing what sets them off so you can avoid them. Other preventive strategies include getting enough sleep, drinking enough water, reducing stress, and cutting down on coffee and alcohol.
In addition, if you have specific warning signals, it’s important to consult a doctor so they can rule out any underlying health concerns that might be causing your recurrent migraines. Chronic migraines may have varying effects on different people, so it’s important to tailor your therapy accordingly. Treatment and preventative strategies may help people with chronic migraines lead more productive lives and lessen the toll it has on their health and happiness.