A Comprehensive Guide to Understanding Varicocele
Are you suffering from varicocele in silence? Don’t worry, this comprehensive guide on varicocele has everything covered.
From aching discomfort to fertility issues, this guide uncovers symptoms, causes and proven treatment options that can help you take control of your health and well-being.
What is a Varicocele?
Definition and Overview
Varicocele is the enlargement of the veins in the scrotum. It is similar to varicose veins seen in the legs.
Varicocele develops when the vein valves fail, allowing blood to pool and enlarge the veins, disrupting the testicular temperature, hormone production, and sperm quality.
Prevalence and Who is Affected
15%-20%(1) of men suffer from varicocele. Apart from this, upto 40% males are infertile(2).
Although it is common on the left side due to anatomical differences in venous drainage, 10% of men have reported bilateral varicocele(3).
What Causes Varicocele in Men?
Valve Dysfunction in Testicular Veins
The primary cause of varicocele is a defective venous valve, which hinders proper blood drainage, resulting in the pooling of blood and vein enlargement in the scrotum.
Risk Factors: Genetics, Puberty, Physical Activity
- Genetic predisposition for weak venous valve
- Rapid growth during puberty causes the inability to handle the increased blood flow.
- Prolonged standing hours or heavy physical activity may increase the symptoms or reveal inactive varicoceles.
Types and Classification of Varicocele
Varicoceles are graded to classify their size and how easily they can be identified during the examination, aiding in diagnosis and treatment planning.
Grading Systems (Based on Size and Palpability)
The following is the common grading system:
1) Grade I: Small, not visible, only palpable with Valsalva manoeuvre.
2) Grade II: Palpable without Valsalva, not visible.
3) Grade III: Large, visible bulging veins
Etiological Classifications
Primary Varicocele:
The most common type usually develops during puberty; its exact cause is unknown, though factors like faulty valves in the veins are suspected.
Secondary Varicocele:
Caused by an obstruction in the veins of the abdomen, which can be a symptom of other conditions.
What are the Signs and Symptoms Associated with Varicocele?
The condition is mostly asymptomatic.
Many men may not even be aware that they are suffering from the condition until they undergo a checkup related to infertility or a routine examination.
The following are the noticeable symptoms:
Swelling or “Bag of Worms” Appearance
This is a classical symptom of varicocele, where the soft mass appears or feels like a bag of worms, often more pronounced while standing.
Dull or Severe Pain, Heaviness in Scrotum
Mild or severe pain can result from a varicocele. Many patients complain of “aching” sensations that are often associated with long hours.
Varicocele can cause severe pain if there is blood clotting and inflammation. Leading to blood pooling and, hence, the pain.
Patients with scrotal pain should be evaluated through scrotal ultrasonography to rule out any underlying pathology and a urine test for any infection.
Testicular Atrophy and/or a Lump
Reduced testicular size (atrophy) and a lump may indicate chronic varicocele.
Fertility Issues
Varicocele may result in low sperm count, poor motility, and abnormal morphology, making it a leading cause of male infertility.
What are the Complications of Varicocele?
Infertility: Sperm Count, Motility, and Quality
Varicocele can cause impaired fertility, low testosterone production by the testis.
In some cases, patients may also experience azoospermia, or the complete lack of sperm in the ejaculate.
By raising scrotal temperature and disrupting blood flow, varicocele negatively affects sperm production and function.
Testicular Atrophy
Inadequate blood flow and increased pressure can shrink the affected testicle over time.
Rare: Venous Thrombosis, Embolism, and Psychological Impact
Though uncommon, thrombosis, venous embolism, and psychological distress due to infertility or chronic discomfort can also occur.
How to Diagnose Varicocele?
There are multiple ways to diagnose varicocele. The following are the steps you can follow:
- Patient’s History and Physical Examination:
Initial diagnosis begins with a detailed medical history and physical examination.
- Inspection and Palpation (Standing and Lying Down):
The doctor examines the patient while standing and lying. The patient is asked to perform a Valsalva manoeuvre to enhance vein visibility.
- Valsalva Manoeuvre:
The patient is instructed to bear down (as if blowing into a balloon), increasing abdominal pressure and accentuating the varicocele for detection.
- Imaging:
- Scrotal Ultrasound: Confirms the diagnosis by visualising dilated veins
- Doppler Studies: Assess blood flow and reflux within the veins
Role of Laboratory Tests
In cases of infertility, semen analysis and hormonal panels (FSH, LH, testosterone) are performed to assess reproductive function.
What are the Management and Treatment Options?
The varicocele treatment is primarily based on the extent of the symptoms and desires of fertility, in addition to the general health of the patient.
Although not all varicoceles need treatment, it is necessary to treat them in some situations to preserve the functioning of the testicles, to eliminate pain, or to overcome infertility.
Watchful Waiting for Asymptomatic Cases
Varicoceles are often detected accidentally during a regular physical examination or assessment of other issues.
Treatment may not be needed in cases where the patient has no pain, testicular shrinkage and fertility problems. Instead, a watchful waiting strategy is implemented.
This involves:
- Consistency to check up with a urologist
- Checking the size of the testicles and sperm vitality (the sperm and fertility issue)
- Lifestyle modification to reduce venous pressure (e.g. keeping off long periods of standing time, wearing supportive undergarments)
Indications for Treatment
The requirement of the treatment depends on the condition, especially if it is symptomatic, hinders day-to-day function or affects testicular health.
The main indications include:
- Dragging or constant pain in the scrotum that obstructs day-to-day functions
- Atrophy of the testicles in young patients indicates poor testicular health.
- Male factor infertility, especially when the semen analysis indicates reduced sperm number, motility or defective morphology
- Cosmetic or psychological discomfort, though less common, may also influence treatment decisions.
What are the Surgical Treatment Options?
Surgery aims to ligate or block the affected vein and redirect the blood flow to a healthier one, thereby relieving the pressure.
- Microsurgical Varicocelectomy
The gold standard of varicocele repair
This is done under an operating microscope, and each abnormal vein can be identified and ligated accurately, with lymphatics and arteries preserved.
Has a low recurrence rate and the least risk of complications
Performed under local or general anaesthesia, the patient does not have to stay admitted until complete recovery.
- Laparoscopic Varicocelectomy
Keyhole surgery, which involves small incisions in the abdomen, is performed together with camera-guided surgery under general anaesthesia.
It is faster to recover than open surgery, with slightly more recurrence and complication rates than microsurgery and may be used preferably in bilateral varicoceles or situations requiring abdominal exploration.
- Open Surgery (Inguinal or Retroperitoneal Approach)
A conventional surgical approach, which is nonetheless applied in certain centres where the capability of microsurgery is lacking
It is associated with greater dissection and risks of complications, including hydrocele development or destruction of adjacent structures.
Usually takes longer to heal.
Source:ncbi(4)
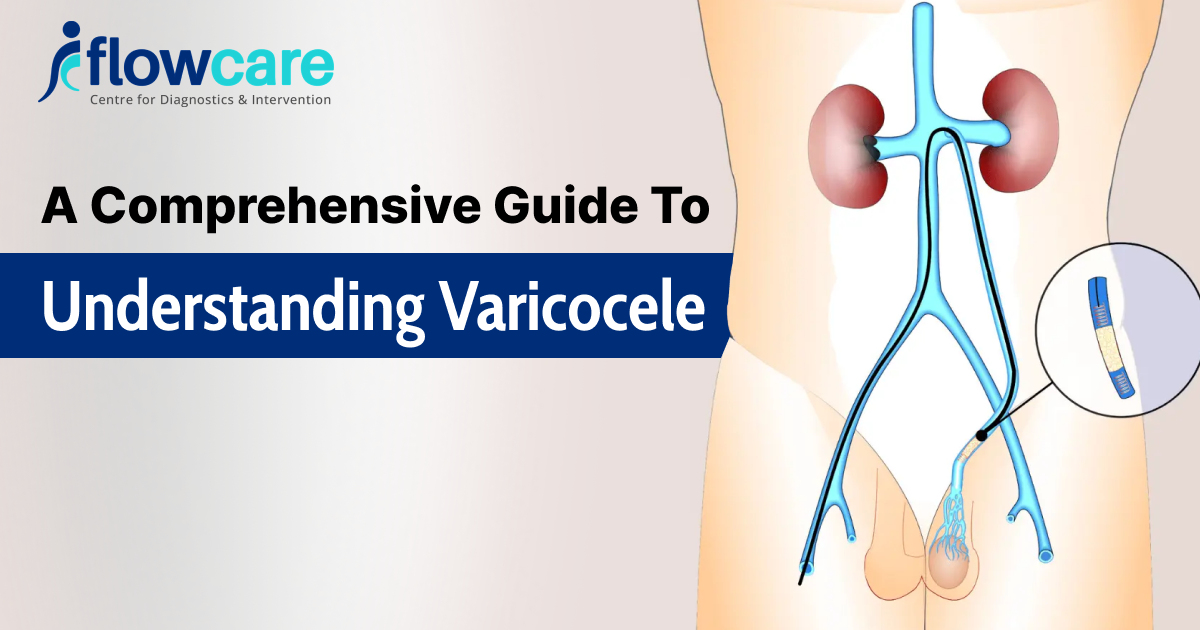
What are Non-Surgical/Interventional Treatments for Varicocele?
Varicocele embolisation is a procedure that involves less invasiveness and is assisted by imaging, and is done by a radiologist.
It involves inserting a catheter into a vein ( in the groin or neck).
The catheter is then directed to the leaking testicular vein and fills it with coils or sclerosing substances to block it, thus preventing back flow.
No cutting or sewing required
The recovery time is short – most patients start their normal activities within 24 hours.
Varicocele embolisation is especially useful for individuals who are not willing to go for surgery, who are seeking for army enrollment or have a recurrence of varicocele even after multiple surgical interventions.
Recovery and Prognosis of Varicocele
The duration of recovery differs according to the treatment procedure.
Most men can resume light work after 2-3 days and complete physical activity after 1-2 weeks.
Pain relief is usually observed a week or even days following the surgery.
A gradual improvement in semen parameters (sperm count, motility, morphology) often noticed 3 to 6 months after the treatment, but the extent depends on the particular person.
Remedy of fertility in men with fertility problems can remarkably enhance the possibility of natural conception or better results in the assisted reproductive techniques (ART).
What are the Complications and Risks of Treatment
The following complications might occur during the treatment:
- Recurrence of varicocele
- Hydrocele, fluid formation around the testicles
- Accidental injury to the testicular artery
- Infection or delayed healing
Lifestyle Modification to Prevent and Manage Varicocele
The following lifestyle changes can be done:
- Stay active and maintain a healthy weight to prevent intra-abdominal pressure.
- Avoid long-standing hours and heavy weight lifting
- Use supporting undergarments to reduce discomfort during daily activities
- Avoid hot temperatures, for example, steam baths, as they can affect sperm count and health
Conclusion
Varicocele is a very common condition that may impair testicular health and fertility; however, it can be handled through proper care.
Early diagnosis and professional advice may assist you in safeguarding your reproductive health and lead a comfortable life through watchful observance or complex therapy.
When necessary, consult a specialist and do not leave the signs without attention.
FAQs
Can a varicocele affect both testicles?
Usually, due to anatomical differences, the left side is affected, but in a few cases, both testicles are affected.
Doesa varicocele always cause infertility?
Not always is fertility the issue in many men suffering from varicocele. But the condition remains one of the leading causes of reversible male fertility.
Is recurrence common after the treatment of varicocele?
Recurrence rate is much lower with varicocele embolization.
Are lifestyle changes enough to prevent complications?
Lifestyle changes can only reduce the discomfort but not cure or reverse varicocele. Medical evaluation and proper treatment are essential for long-term outcomes.