Inferior Vena Cava (IVC) Filter
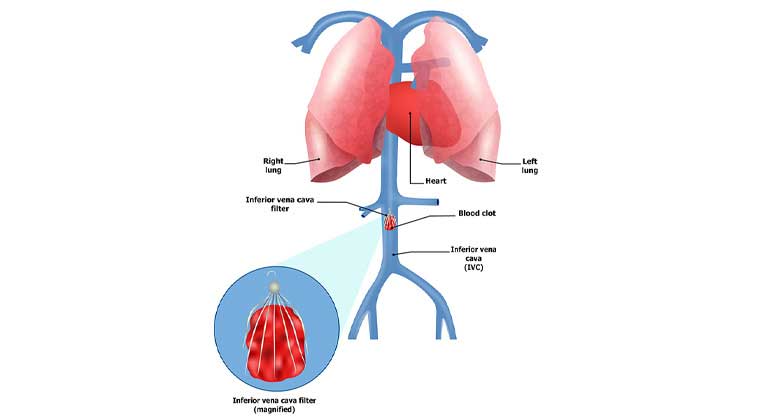
Deep vein thrombosis is a condition in which the blood thickens and clumps together forming a blood clot, in most cases, in the deep veins of the thigh or lower legs. Along with other complications, DVT can lead to a serious life-threatening medical condition such as Pulmonary Embolism in which a deep blood clot (thrombus) breaks free and travels with the blood and gets stuck in a vessel in the lung.
Placement of IVC filter or Inferior Vena Cava filter is the most common low-risk procedure for Pulmonary Embolism prevention.
Indications are high-risk pelvic surgery, Ileocaval thrombosis, recently operated cases in which thrombolytics cannot be given, failed anticoagulation.
Inferior Vena Cava is a major vein that carries blood from lower body parts back to the heart. IVC filter, a small wiry device, is placed in the Inferior Vena Cava so that the blood passes through it. This filter then catches and stops the blood clots from moving up further and thus helps in preventing Pulmonary Embolism.
Under imaging guidance and local anesthesia, the Interventional Radiologist inserts a catheter into the vein through a pinhole skin incision (cut) and gently moves it into the IVC. Upon proper placement, a collapsed IVC filter is sent through the catheter and the filter is then left in place and the catheter is removed. The filter expands and attaches itself to the walls of the vein (IVC). Once the IVC filter is in place, it filters the blood and catches any blood clots.
After a successful IVC filter placement, the patient can be discharged on the same day if everything remains normal. However, follow-ups/check-ups at regular intervals are recommended to ensure the proper dose of anticoagulation. Generally IVC Filter is removed after 3-6 months of placement.
Catheter-directed Thrombolysis
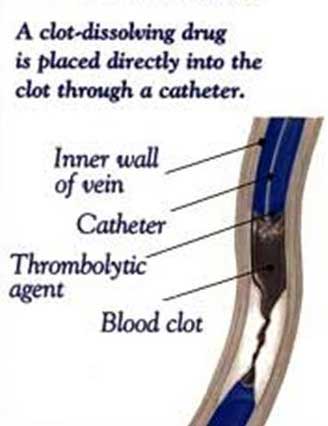
Catheter-directed Thrombolysis (CDT) is a minimally-invasive endovascular (inside the blood vessel) treatment to treat vascular blockages and improve blood circulation by dissolving abnormal blood clots. Usually performed under moderate sedation (Local anaesthesia) by an expert Specialist Interventional Radiologist with the help of real-time imaging, the aim of this procedure is to deliver clot-dissolving medications (thrombolytics) essentially within the blood clot.
After confirming the blood vessel and the area having poor blood circulation with prior imaging, under x-ray guidance, a catheter is inserted through the skin into the blood vessel and moved forward to the area of poor circulation. Upon further confirming the blood clot through contrast injection and x-ray images, thrombolytic (clot-dissolving) medication is delivered through the catheter directly within the blood clot over several hours to a few days, however, most clots dissolve within 24 hours. During this period, the patient is kept under close monitoring. Upon completion of the procedure, the patient is discharged with pain medication.
A follow-up visit with Interventional Radiologist for a physical check-up, imaging and blood test is recommended.
Mechanical Thrombectomy
A safer and minimally-invasive alternative or adjunct (supportive) treatment to the use of thrombolytic medication-based procedures is Mechanical Thrombectomy. This procedure entails the removal of blood clot from the patient’s artery with the use of specialized equipment by an expert Interventional Radiologist.
Due to its high success rate, along with DVT, Mechanical Thrombectomy is also extremely useful in the treatment of the following life-threatening conditions:
Acute Ischemic Stroke – An extremely life-threatening condition in which the blood supply to the brain is obstructed/blocked by a blood clot in the arteries supplying blood to the brain (internal carotid and vertebral arteries). The clot can either form in the arteries supplying the blood to the brain or in an artery in another area and then travel with the blood to those arteries. Only a few minutes of blood supply disruption can result in permanent brain damage and even death.
Acute Limb Ischemia – Another life threatening condition due to blockage in peripheral or limb vessels, is Acute Limb Ischemia. In simple words, this condition occurs due to a rapid decrease in blood flow to the limbs because of occlusion of the peripheral artery (which supplies blood to the limbs). Unless quick and appropriate treatment is administered, this can result in amputation of the limb (extremity).
All the above conditions can be caused by blood clots blocking the supply of blood in the arteries.
Under continuous X-ray or fluoroscopy monitoring, the Interventional Radiology Specialist inserts a thread-like catheter into the artery through a small incision (cut) in the skin. This catheter is then advanced under imaging guidance through the artery to the clot. After confirming the correct catheter placement, a tiny net-like device (stent retriever) is pushed through the clot. This stent retriever captures the clot and then the doctor pulls it out backward, thereby removing the clot completely.
Mechanical Thrombectomy is a cost-effective, relatively quick procedure, usually taking an expert Interventional Radiologist less than an hour or two. The recovery period after Mechanical Thrombectomy is very fast and the patient recovers on the table in case of Acute Stroke while in case of DVT or Acute Limb Ischemia, the recovery time is 1-2 days.