Exploring the Link Between Trigeminal Neuralgia and Facial Pain
Facial pain can be debilitating, affecting one’s quality of life and daily functioning. Among the myriad of conditions contributing to facial pain, trigeminal neuralgia stands out as one of the most excruciating. Trigeminal neuralgia is characterized by sudden, severe facial pain originating from the trigeminal nerve, often triggered by mundane activities such as eating, talking, or even touching the face lightly. Understanding the link between trigeminal neuralgia and facial pain is crucial for effective diagnosis and treatment. Facial pain, when chronic and severe, can disrupt daily life and challenge even the most resilient individuals. Trigeminal neuralgia, a condition often associated with intense facial pain, sheds light on the intricate relationship between neurological disorders and the perception of pain. Understanding this link is crucial for both patients and healthcare providers to effectively manage and alleviate the debilitating symptoms associated with trigeminal neuralgia.
What is Trigeminal Neuralgia?
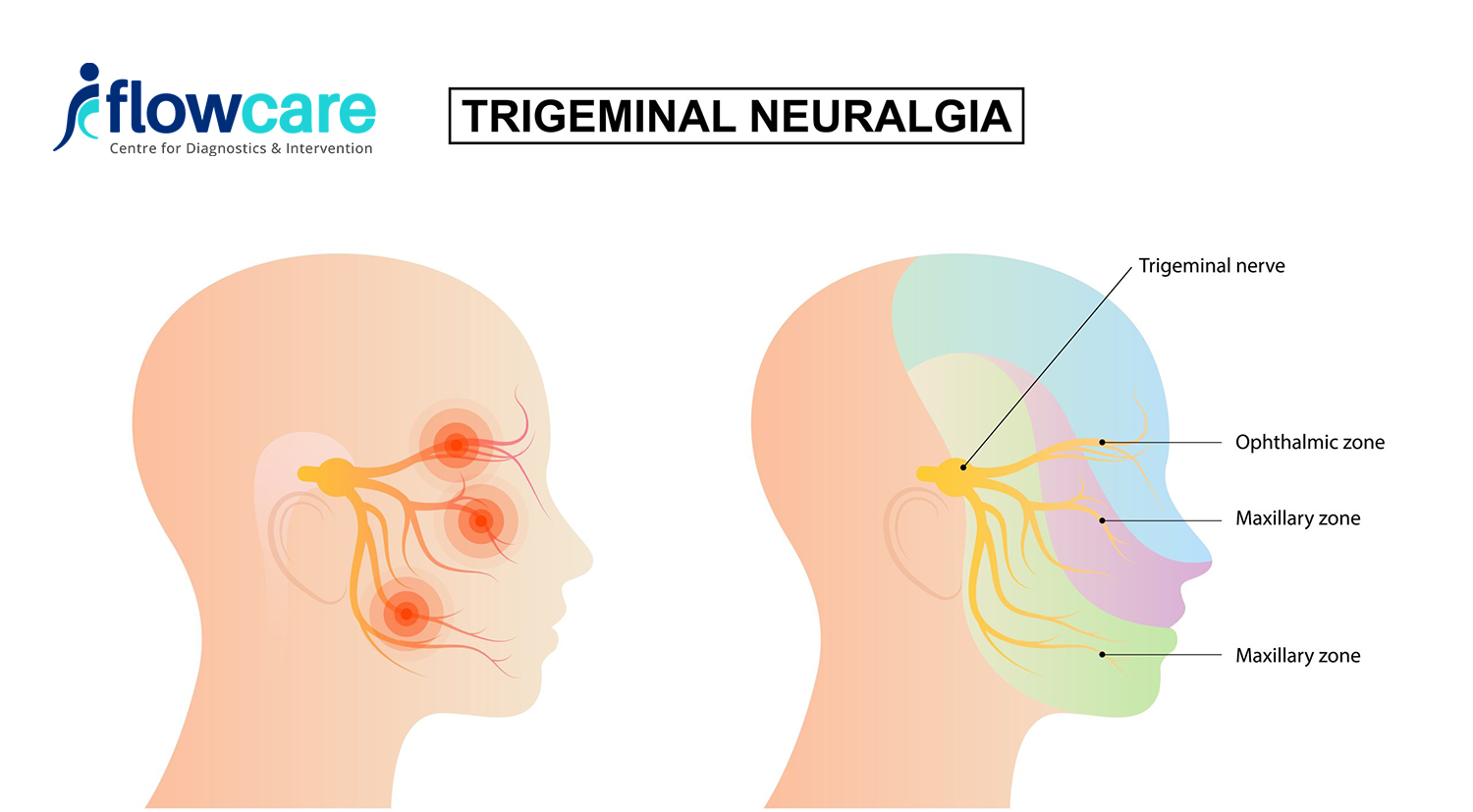
The trigeminal nerve, also known as the fifth cranial nerve, is responsible for transmitting sensations from the face to the brain. Trigeminal neuralgia is a disorder characterized by sudden, intense facial pain due to dysfunction or damage to this nerve. The pain is often described as stabbing, shooting, or electric shock-like, and can be triggered by trivial stimuli such as a gentle breeze or a light touch.
Symptoms of Trigeminal Neuralgia
Patients with trigeminal neuralgia typically experience episodes of intense pain in specific areas of the face, often around the eyes, nose, lips, scalp, forehead, and jaw. The pain can be brief, lasting from a few seconds to a couple of minutes, but can occur repeatedly throughout the day, significantly impacting daily activities and overall well-being. Some individuals may also experience continuous, dull aching or burning sensations between episodes of acute pain.
Understanding Facial Pain:
Facial pain is a complex and often distressing condition that can significantly impact a person’s quality of life. From sharp, stabbing sensations to dull, persistent aches, facial pain can manifest in various forms and intensities, making it crucial to understand its underlying causes, symptoms, and available treatment options.
Causes of Facial Pain:
Facial pain can arise from a multitude of factors, ranging from dental problems to neurological disorders. Some common causes include:
- Dental Issues: Tooth decay, gum disease, or dental abscesses can lead to localized pain in the jaw, gums, or teeth.
- Sinus Infections: Inflammation or infection of the sinuses can cause facial pressure, pain around the eyes, cheeks, or forehead, and nasal congestion.
- Temporomandibular Joint (TMJ) Disorders: Dysfunction of the TMJ, which connects the jawbone to the skull, can result in jaw pain, clicking or popping sounds, and difficulty chewing.
- Trigeminal Neuralgia: A disorder of the trigeminal nerve, trigeminal neuralgia causes sudden, severe facial pain that can be triggered by even mild stimuli such as touching the face.
- Migraine: Some individuals experience facial pain as part of a migraine headache, often accompanied by other symptoms such as nausea, sensitivity to light, and visual disturbances.
- Nerve Damage: Injuries or compression of facial nerves can lead to neuropathic pain, characterized by burning, tingling, or electric shock-like sensations.
Symptoms of Facial Pain:
The symptoms of facial pain can vary depending on the underlying cause but may include:
- Sharp, Stabbing Pain: Sudden, intense pain that comes and goes, often described as stabbing or shooting.
- Dull, Aching Sensations: Persistent, throbbing pain that may worsen with movement or pressure.
- Facial Numbness or Tingling: Loss of sensation or abnormal tingling sensations in the face.
- Headaches: Pain that radiates from the face to the head, often accompanied by other migraine symptoms.
- Difficulty Eating or Speaking: Pain or discomfort that interferes with normal activities such as eating, talking, or smiling.
The Trigeminal Nerve and Facial Sensation
The trigeminal nerve, the largest of the cranial nerves, plays a fundamental role in facial sensation. It consists of three branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3), each responsible for innervating specific areas of the face, including the eyes, nose, lips, scalp, forehead, and jaw.
When functioning correctly, the trigeminal nerve efficiently transmits sensory information from these areas to the brain, allowing us to perceive touch, temperature, and pain. However, in individuals with trigeminal neuralgia, the nerve becomes hypersensitive or undergoes compression, leading to abnormal firing of pain signals and the characteristic episodes of excruciating facial pain.

Symptoms and Triggers of Trigeminal Neuralgia
The hallmark symptom of trigeminal neuralgia is intense, episodic facial pain, typically localized to one side of the face. The pain can be triggered by various stimuli, including:
- Light touch or pressure on specific areas of the face
- Chewing, talking, or brushing teeth
- Exposure to cold air or wind
- Eating or drinking hot or cold foods
These triggers can vary among individuals and may change over time, complicating the management of trigeminal neuralgia.
The Complex Nature of Facial Pain
Facial pain, including that associated with trigeminal neuralgia, is multifaceted and influenced by a myriad of factors, including neurological, vascular, and psychological components. While trigeminal neuralgia primarily affects the sensory function of the trigeminal nerve, other conditions such as temporomandibular joint disorders (TMJ), sinus infections, or dental problems can also contribute to facial pain.
Furthermore, the perception of pain is highly subjective and can be influenced by emotional, cognitive, and environmental factors. Chronic facial pain not only impacts physical well-being but can also lead to emotional distress, social isolation, and impaired quality of life.
Treatment Strategies for Trigeminal Neuralgia and Facial Pain
Managing trigeminal neuralgia and facial pain requires a comprehensive approach tailored to the individual needs of each patient. Treatment options may include:
- Medications: Anticonvulsants, muscle relaxants, and antidepressants are commonly prescribed to alleviate pain and reduce nerve irritation.
- Interventional Procedures: Techniques such as radiofrequency ablation (RFA), nerve blocks, or botox injections may be used to interrupt pain signals and provide relief.
- Surgery: In severe cases or when conservative treatments fail to provide adequate relief, surgical procedures such as microvascular decompression (MVD) or gamma knife radiosurgery may be considered to alleviate nerve compression.
Conclusion
Trigeminal neuralgia exemplifies the intricate relationship between neurological disorders and facial pain. By understanding the underlying mechanisms and triggers of trigeminal neuralgia, healthcare providers can develop tailored treatment plans to alleviate pain and improve the quality of life for affected individuals. Through ongoing research and advancements in medical technology, there is hope for more effective treatments and better outcomes for those living with trigeminal neuralgia and other facial pain disorders.